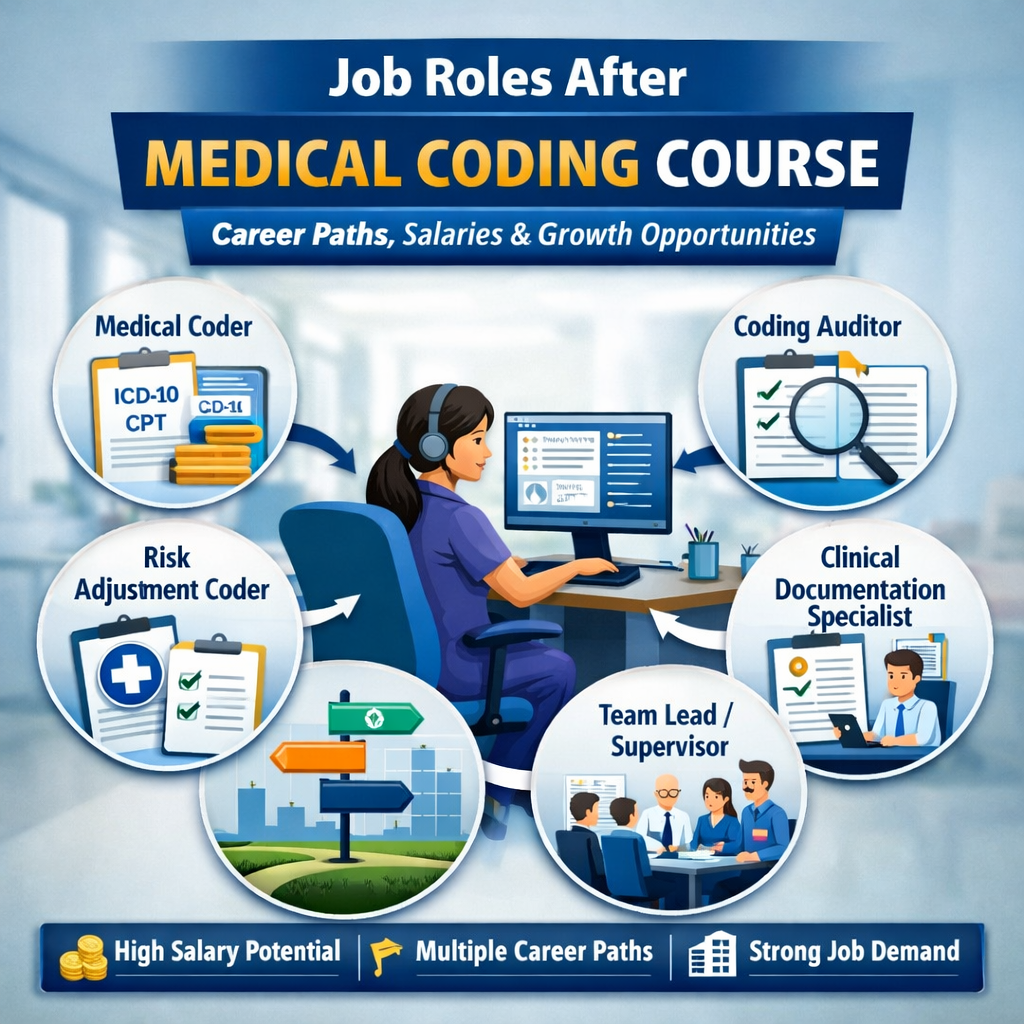
Job Roles After Medical Coding Course: Career Paths, Salaries, and Growth Opportunities
The healthcare industry runs on accuracy, compliance, and structured clinical data. Behind every insurance claim, patient record, and hospital reimbursement process is a trained medical coding professional ensuring that healthcare services are translated correctly into standardized codes.
As healthcare systems expand globally—and particularly with the growth of medical billing and revenue cycle outsourcing—medical coding has evolved into a long-term, multi-role career pathway, not just an entry-level job.
For learners completing or considering a medical coding course, one of the most common questions is:
“What are the job roles after a medical coding course, and how far can this career take me?”
The answer is encouraging. Medical coding offers clear progression paths, role specialization, leadership opportunities, and strong demand across hospitals, insurance companies, healthcare BPOs, and audit firms.
Training institutions like Transorze prepare learners for this progression through industry-aligned curricula, hands-on coding practice, and certifications recognized by national and academic bodies.
This article explores five key job roles after a medical coding course, explaining responsibilities, skills required, salary expectations, and long-term career growth—while also showing how structured training prepares you for each role.
Why Medical Coding Offers Strong Career Progression
Medical coding is governed by globally accepted standards such as:
- ICD-10-CM/PCS for diagnoses and procedures
- CPT for outpatient and physician services
- HCPCS Level II for supplies and non-physician services
Because accuracy directly impacts patient safety, legal compliance, and hospital revenue, experienced coders are always in demand. As professionals gain expertise, they naturally move into higher-responsibility roles such as auditing, documentation improvement, risk adjustment, and team leadership.
Transorze’s medical coding programs are designed to reflect these real-world career ladders, supported by skill-based certification frameworks under NSDC and vocational recognition aligned with UGC – NCVET, along with academic pathways through Medhavi University.
1.Medical Coder – The Foundation Role
Role Overview
The Medical Coder is typically the first and most essential role after completing a medical coding course. Medical coders convert clinical documentation—such as physician notes, operative reports, discharge summaries, and lab results—into standardized medical codes.
These codes determine:
- Insurance reimbursement
- Statistical reporting
- Compliance with healthcare regulations
Key Responsibilities
- Review patient medical records for completeness
- Assign accurate ICD-10, CPT, and HCPCS codes
- Ensure coding aligns with payer guidelines
- Identify documentation gaps and query providers
- Maintain productivity and accuracy benchmarks
Skills Required
- Strong understanding of anatomy, physiology, and medical terminology
- In-depth knowledge of coding guidelines
- Attention to detail and compliance awareness
- Basic understanding of revenue cycle management
- Ability to work with EHR and coding software
Salary Expectations (India)
- Entry-level: ₹2.5 – ₹4 LPA
- With 2–4 years’ experience: ₹5 – ₹7 LPA
Career Growth
Medical coders often progress into:
- Senior Medical Coder
- Specialty Coder (e.g., inpatient, outpatient, surgical)
- Coding Auditor or Risk Adjustment Coder
How Transorze Prepares You
Transorze’s medical coding curriculum emphasizes:
- Extensive ICD-10, CPT, and HCPCS coding practice
- Real-world case studies and charts
- Compliance-based coding scenarios
- Industry-aligned assessments recognized under NSDC frameworks
2.Coding Auditor – Ensuring Accuracy and Compliance
Role Overview
A Coding Auditor reviews coded medical records to ensure accuracy, compliance, and adherence to regulatory guidelines. This role is critical in minimizing claim denials, audits, and legal risks.
Auditors are typically experienced coders who understand both clinical documentation and payer regulations.
Key Responsibilities
- Audit coded charts for accuracy and completeness
- Identify coding errors and compliance risks
- Provide feedback and training to coders
- Support internal and external audits
- Monitor adherence to ICD-10, CPT, and payer rules
Skills Required
- Advanced knowledge of coding guidelines
- Strong analytical and investigative skills
- Understanding of payer policies and compliance rules
- Communication and reporting skills
- Ability to mentor and guide coding teams
Salary Expectations
- Mid-level: ₹6 – ₹9 LPA
- Senior auditors: ₹10+ LPA
Career Growth
Coding auditors can advance into:
- Compliance Manager
- Revenue Integrity Specialist
- Healthcare Quality Analyst
How Transorze Prepares You
Through advanced coding modules and quality-focused training, Transorze builds the accuracy mindset required for auditing roles. Learners trained under vocational standards aligned with UGC-NCVET gain strong credibility in compliance-driven roles.
3.Risk Adjustment Coder – Supporting Value-Based Healthcare
Role Overview
A Risk Adjustment Coder plays a key role in value-based care models by ensuring that patient diagnoses are accurately coded to reflect disease severity and chronic conditions.
This role is especially prominent in insurance and payer organizations.
Key Responsibilities
- Review medical records for chronic and complex conditions
- Assign ICD-10 codes impacting risk scores
- Ensure accurate Hierarchical Condition Category (HCC) coding
- Support payer reimbursement accuracy
- Identify documentation gaps
Skills Required
- Deep ICD-10 expertise
- Understanding of HCC models
- Knowledge of clinical documentation standards
- Analytical thinking and attention to detail
Salary Expectations
- Entry-to-mid level: ₹6 – ₹8 LPA
- Experienced professionals: ₹10 – ₹12 LPA
Career Growth
Risk adjustment coders often move into:
- Risk Adjustment Auditor
- Clinical Documentation Specialist
- Healthcare Analytics roles
How Transorze Prepares You
Transorze integrates risk adjustment concepts into advanced coding training, helping learners understand how coding impacts population health, payer models, and reimbursement outcomes.
4.Clinical Documentation Specialist – Bridging Clinical and Coding Teams
Role Overview
A Clinical Documentation Specialist (CDS) works closely with physicians to improve the clarity, completeness, and accuracy of clinical documentation.
This role directly influences coding quality, patient safety, and hospital revenue.
Key Responsibilities
- Review clinical documentation for clarity and accuracy
- Query physicians for missing or unclear information
- Educate providers on documentation standards
- Support coding and audit teams
- Improve clinical quality metrics
Skills Required
- Strong clinical knowledge
- Advanced medical terminology
- Communication and interpersonal skills
- Understanding of ICD-10 and compliance requirements
Salary Expectations
- Mid-level: ₹7 – ₹10 LPA
- Senior roles: ₹12+ LPA
Career Growth
CDS professionals can advance into:
- CDI Manager
- Clinical Quality Analyst
- Healthcare Compliance Lead
How Transorze Prepares You
Through integrated clinical and coding education backed by Medhavi University academic recognition, Transorze equips learners to transition into documentation-focused roles.
5.Coding Team Lead – Leadership and Management Role
Role Overview
A Coding Team Lead manages teams of coders, ensuring productivity, quality, and compliance. This role combines technical expertise with leadership responsibilities.
Key Responsibilities
- Manage daily coding operations
- Monitor accuracy and productivity metrics
- Train and mentor team members
- Coordinate audits and compliance reviews
- Act as a bridge between management and coders
Skills Required
- Strong leadership and communication skills
- Advanced coding knowledge
- Performance management abilities
- Problem-solving and decision-making skills
Salary Expectations
- Team Lead: ₹8 – ₹12 LPA
- Senior leadership roles: ₹15+ LPA
Career Growth
Coding team leads often move into:
- Coding Manager
- Revenue Cycle Manager
- Healthcare Operations Leadership
How Transorze Prepares You
Transorze’s structured learning pathways, industry exposure, and certification-backed credibility help learners progress into leadership roles with confidence.
Why Transorze Stands Out in Medical Coding Education
Transorze combines:
- Industry-aligned medical coding curriculum
- NSDC-recognized skill training
- Academic pathways through Medhavi University
- Vocational recognition aligned with UGC-NCVET
- Career-oriented role preparation
This ensures learners are not just certified—but job-ready and future-ready.
Conclusion: Building a Long-Term Career After a Medical Coding Course
Medical coding is not a single-job career—it is a structured professional pathway with opportunities in compliance, auditing, documentation, analytics, and leadership.
By choosing the right training provider and understanding the job roles after a medical coding course, learners can plan their careers with clarity and confidence.
With industry-recognized certifications, role-specific preparation, and a strong reputation in healthcare education, Transorze provides the foundation needed to grow from an entry-level coder into a healthcare documentation professional with long-term stability and advancement.
FAQ's
Common job roles include Medical Coder, Coding Auditor, Risk Adjustment Coder, Clinical Documentation Specialist, and Coding Team Lead.
Entry-level medical coders typically earn ₹2.5–4 LPA, with experienced professionals earning ₹6–10+ LPA.
Industry-recognized certifications such as CPC, CCS, and CCS-P enhance employability and career growth.
Transorze offers industry-aligned training with NSDC recognition, academic pathways through Medhavi University, and vocational alignment with UGC-NCVET.
Medical coders assign codes, while coding auditors review coded records for accuracy, compliance, and quality.
Key skills include medical terminology knowledge, coding guideline expertise, attention to detail, and compliance awareness.
With proper training and certification, many learners secure entry-level roles within 3–6 months.
Yes, Transorze programs are aligned with NSDC, Medhavi University, and UGC-NCVET frameworks, making them widely recognized.
